ABO - H - Le - Se
It is quite a surprise how complicated the generation of the blood groups ABO, H, and Le presents itself.
The SE gene does not determine a particular blood group, but whether or not the blood group antigens are secreted in the body fluids (seminal fluid, saliva). In other words, whether the individual is a secretor or not. The ratio of secretors to non-secretors is 80:20.
I start with the ABO blood group because it is clinically the most important.
ABO:
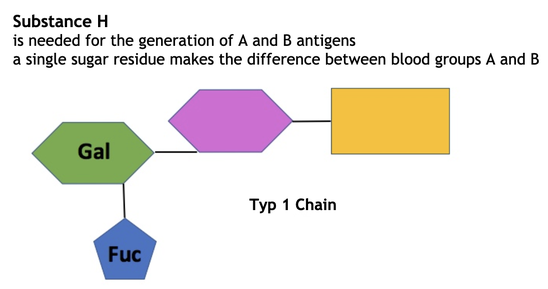
The ABO system relies on substance H as its primary building unit. The generation of substance H requires one of two carbohydrate chains - type 1 and type 2.
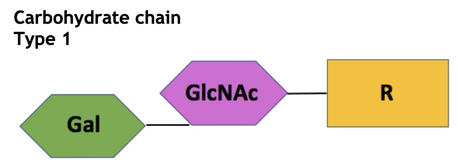

The two chains must first have a fucosyl residue attached before they become the H substance and can be converted into the A or B antigens. Chain 1 is found floating freely in the body fluids and plasma, where it is present as a glycolipid. It can be converted into the soluble substance H by FUT2 (fucosyltransferase 2/Se gene) by attaching a fucosyl group to galactose.
In contrast, chain 2 is bound to the cell membrane of the erythrocytes and must be changed by FUT1 (H gene) to the H substance.
Only when these reactions have taken place can the enzymes that form A and B antigens take effect. The blood group A gets the galactosaminoglycan, and the B group has the galactose attached.
Substance H is thus converted into the blood group antigens. The lowest amount of substance H is found on the erythrocytes of BG A1 because this is almost entirely converted into the A antigen. BG O has only substance H.


Individuals who are HH of the Hh, can form substance H.
Those with two mutant H Alelle - hh - cannot form substance H and, therefore, cannot form ABO blood group antigens.
To make the situation a little more complicated for the patient and the transfusion specialist, these individuals form a naturally strong isoagglutinin against substance H, which means they may only be transfused with blood that does not express substance H - the so-called Bombay type.
(Fortunately, this is very rare, and the patients with this phenotype are mainly found near Mumbai/India).
The SE gene codes for FUT2, which can make the H substance from chain 1. Only about 20% of people have two inactive alleles for this transferase (sese). These individuals cannot convert chain 1 in the plasma into factor H and therefore have no blood group antigens in their body fluids.
LE - SE
The LE gene also codes for fucosyltransferase (FUT3), and the SE gene is the secretor gene (80% have it).
But because with all the upper/lower case letters, overlong enzyme names, and just the dangerous " proximity" to chemistry, most of us just skip over such parts, I'll try something like Dr. Joe - if it's funny enough, it can't be that boring.
So I'll try to explain it with an example. And for simplicity's sake, I'll use BG O:
The enzyme of the LE gene is FUT3, a lovely little unobtrusive enzyme that will keep out of the way of conflict immediately.
The enzyme of the SE gene, the FUT2 is the exact opposite of this - it has to be first everywhere, pushes itself forward and is almost territorial.
And here's what happens:
- both enzymes fight to change the type 1 chain by binding a fucosyl:
- the Le enzyme produces a Lea
- the Se enzyme, the substance H
However, since the Se gene is so much more effective, there are vast amounts of substance H and very little Lea. However, this happens when chain 1 is caught first by the LE gene: it cannot be converted any further and remains a Lea. This is what happens with blood group O.
Let's try the scenario with the other blood groups (AO, AA or BO, BB or AB):
The glycosyltransferase responsible for generating blood groups A and B has the same unpleasant character as the SE gene - the FUT2. So at first, the type 1 chains are mercilessly transformed into the A or B group. In addition, we have an active Lewis gene and an active secretor gene. Then the SE gene - FUT2 - comes, puts another fucosyl residue on top, and makes the complete substance H/A --> in the case of BG A, it is an A antigen. This all sounds so "one after the other". In reality, everything happens practically simultaneously.
But even if all this has already happened, nothing can stop the small and timid Le enzyme FUT3 from carefully approaching the substance H or A (B), attaching a fucosyl residue to it, and turning the A/B antigen into a Leb antigen. A few chains will escape the SE and get fucosyl residue from FUT3. So with this combination of genes:
- active Le enzyme
- active Se enzyme
the individual has a lot of Leb and very little Lea.

Only a few molecules of Lea and Leb are found on the erythrocytes. Many more type 2 chains float around in the plasma as glycolipids. The Lea and Leb molecules drift in and out of the membrane of the erythrocytes. So it can also happen that when you test the erythrocytes - especially with the substance Lea, you get a negative result.
Thus, only people who have deactivated both le alleles can form antibodies against Lea or Leb.

1. If the type 1 chain is reached first by the Le enzyme (FUT3), it becomes a Lea and can no longer be changed.
2. If the Se enzyme (FUT2) is faster, the type 1 chain becomes substance H, which can then be converted into substance Leb by FUT3.
3. If the type 1 chain is already transformed into an H substance and A antigen, the FUT3 can transform it into Leb or, strictly speaking, ALeb.
4. The same thing happens with the B antigen - it, too, is transformed into BLeb.
The picture is from a great video explaining the Le system. It was made by an American transfusion specialist, D. Joe Chaffin, MD, who runs his website on transfusion medicine - it's a lot better than mine, but he's been running it for decades.
If you have trouble with something - I'm sure it's wonderfully explained there.
The website is called: http://bbguy.org
To make things a little easier to understand, let's look at this table:

The Le and Se gene decides which enzymes we have.
1. In the first example, I have FUT2 and FUT3 and, therefore, much more Leb than Lea and am a secretor.
2. In the second example, I only have FUT3 and can only make Lea, which is also found in the body fluids.
3. My Le gene is inactive in the third example, so I have neither Lea nor Leb.
And the exciting thing is that the Lea and Leb substances float around in the plasma and are in constant exchange with the cell membranes of the erythrocytes. This is precisely why babies are born with the Le(a-b-) on the red cells. Only at the age of about six years do they reach the final Lea/b status.
And one last speciality of the Lewis antigens. If red cells with a specific Lewis phenotype are transfused, their phenotype changes relatively quickly (days) into that of the recipient. This is not so surprising when you know that the antigens are taken up from the plasma.
