Blood - fulfils several tasks that can be more or less summarised under the terms "transport & supply". It is a suspension of blood cells - erythrocytes, platelets and leucocytes - in blood plasma. The blood plasma consists of water, proteins, glucose, clotting factors, messenger substances and metabolic waste products. Blood cells are generated in the bone marrow.
Blood donation - in most countries, it is a voluntary and non-remunerated donation of 500 ml of blood, further processed into several blood products. Blood products are considered to be drugs.
Blood donors - women and men between 18 and 70 (the upper age is not precisely defined and is decided individually depending on the health and physical condition of the potential donor) who donate blood voluntarily and free of charge. In some countries, you can donate blood at the age of 16.
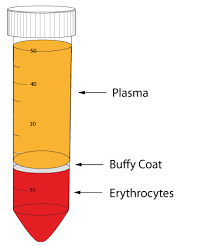
- at the bottom are the erythrocytes
- on top of the erythrocytes is a very narrow layer of leucocytes
- on top is the plasma
- if centrifuged very fast, the platelets will collect just above the white cells in the centre of the tube
- if centrifugation is slow, the platelets remain in the plasma - this is called PRP (Platelet Rich Plasma) or, in the first case PPP (Platelet Poor Plasma)
- to attack and destroy cells directly by forming a water-permeable opening in the cell membrane, causing the cell to burst due to the osmotically inflowing water
- through their activation, some of the complement factors become decoys for further immune cells and binding sites for antibodies and, in this way, are involved in the immune response
Cytokines - Messenger substances that are produced by different cells and thereby either activate or attract other cells
FFP - fresh frozen plasma - after fractionation of whole blood into erythrocytes, thrombocytes and plasma, the plasma obtained is either frozen for direct transfusion as single donor plasma within 24h or sold to the pharmaceutical companies.
Genotype - defines which gene is detectable in an individual by molecular biology. An example of this would be the Rhesus D gene (RHD). A gene can occur in different variants - different alleles. The gene for the Duffy blood group can appear as either FYA or FYB. The genotype can almost always be used to predict the phenotype - but sometimes, the expression of a gene product is suppressed. There can be several causes for this: Single point mutations of the gene itself, null alleles, and mutations in the start sequence of a gene that result in the genetic information not being transcribed into the RNA and, thus, not being expressed.
See also phenotype.
Haemoglobin - the main component of erythrocytes. Transports oxygen to the organs and removes carbon dioxide. The uptake of O2 and the release of CO2 takes place in the lungs.
HLA - Human Leukocyte Antigens - Genes that encode the Major Histocompatibility Complex. These are proteins that are expressed on all human cells and define our immunological identity.
Leukocytes depletion - for over 20 years, white blood cells have been removed from all blood products in Austria by filtration during manufacturing (the maximum permissible cell content of leukocytes is 10^6 cells).
Octaplas - the most common plasma product in Austria. FFP from several hundred donors is pooled, pathogen-inactivated by various procedures and returned to the blood banks as Octaplas.
Phenotype - is, in its simplest form, the appearance of a gene product. If the RHD gene is expressed, the phenotype of the individual will be Rhesus D positive. Taking the Duffy blood group as an example, the gene may be present in the FYA or FYB variant. This gene is present in duplicate (one from the mother and one from the father). If both genes are present in the FYA variant, the phenotype is Fya+ Fyb- or otherwise represented Fy (a+b-). The individual is homozygous for Duffy a. However, if FYA was inherited from the mother and FYB from the father, the phenotype is Fy (a+b+) - heterozygous.
Serum - when blood plasma clots, the fibrinogen precipitates and what remains is serum.
Stemcells - when we talk about stem cells in a therapeutic sense, we usually mean haematopoietic stem cells. They represent a very early developmental group of blood cells, and their "final destination" has not yet been determined. They can develop into all three cell groups: Erythrocytes, Platelets and Leukocytes. They can be obtained in two different ways: by bone marrow puncture or by apheresis. Both methods have advantages and disadvantages, but apheresis is currently more popular because the cells can be collected from the donor relatively easily.
Wholeblood - the term comes from blood donation. It is blood taken directly from a donor, anticoagulated only, but otherwise not further processed. It is rarely used for direct transfusion because transfusion reactions occur much more frequently. But whole blood is experiencing a renaissance, for example, in war zones.
Last update on 08.08.2023.
