BLOOD GROUPING
Blood grouping in compliance with the guidelines includes the following:
- identification of the antigens on the red blood cells
- identification of isoagglutinins (natural antibodies against blood group antigens) in plasma
- the determination of the rhesus factor
- ruling out irregular antibodies
1. ANTIGENS
A tube with EDTA blood is suitable for blood grouping.
In most immunohaematology laboratories, the blood group is determined on an automated system.
In the first step, the patient's erythrocytes are placed in gel cards containing antisera (anti-A, anti-B, anti-AB, anti-D, anti-CDE).

Principle of the gel test:
These wells are approx. 1.5 cm high and 6 of each are joined together to form a card.
A drop of the diluted patient's blood is placed on top and incubated for approx. 20-30 min. at 37°C or RT, depending on the test setting. Afterwards, the cards are centrifuged for 15 min. and analysed.

The higher the number of cells agglutinated by the antibodies present in the wells during incubation, the more difficult it is for them to migrate down the column during centrifugation.
If all cells form a line at the top of the gel, it means that all cells are agglutinated and there is a maximum antibody-antigen reaction.
If all cells are at the bottom of the well, there was no reaction at all and the free erythrocytes were able to migrate down without any problems.
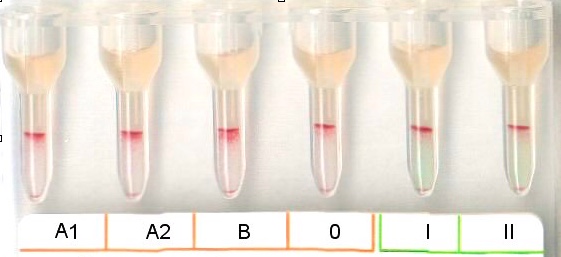
And this is how it looks in practice:
After the cards have been centrifuged, the results can now be read.
In the well with anti-A, the antibodies were not interested in the erythrocytes at all. These went down to the bottom unhindered.
On the other hand, a strong reaction can be seen in the well with anti-B and anti-AB: all the cells were captured and agglutinated by the antibodies and remained on top of the gel.
The same reaction is seen with anti-D and anti-CDE - our patient has the blood group B Rhesus D positive.
2. ISOAGGLUTININS
Even though we already have some information about the patient's blood group, we need more details to rule out rare combinations. Everyone has antibodies against blood group antigens that they don't have. In the case of blood group B, we need to check for isoagglutinins against the A antigen. To do this, we perform a serum reverse typing, where we incubate erythrocytes of blood groups A1, A2, B, and O (previously typed donor cells) with a drop of the patient's serum, and then centrifuge the mixture.
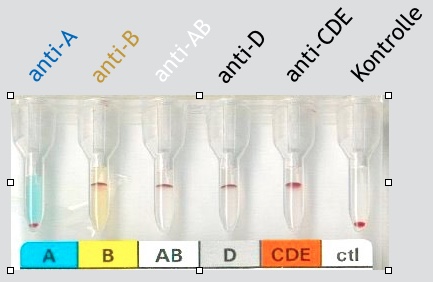
And the result then looks like this:

The cells reacted where an A antigen was present.
(I won't go into more detail about A1 and A2. Both are blood group A, and that's all you need to know, unless you're a transfusion specialist).
We don't see any reaction with the blood group B cells and obviously we don't see any reaction with blood group O cells.
The O blood group cells are actually meant to be the perfect negative control.
An additional task of the O cells is to reveal the Bombay type. Even though most of us do not ever actually get to see the Bombay type in our whole career - it is important to recognise it immediately.
3. RHESUS
More about the Rhesus factor can be found on the separate Rhesus website.
In most cases, the Rhesus factor can already be determined from the antigen identification card.
In our case, it is blood group B and because the well with anti-D also reacted very strongly, there are also D antigens on top of the cells - i.e. Rhesus D positive. The well with the anti-CDE antibody only provides additional information if the anti-D is negative. This is because it is used to check whether there is perhaps a rhesus C or rhesus E in the CDE rhesus formula (for Rh neg ccddee).
4. ANTIBODY SCREENING TEST TO RULE OUT IRREGULAR ANTIBODIES
This test is usually performed using purchased erythrocytes of blood group O. All serologically and molecularly detectable blood group antigens are already determined on these cells, but the package insert mainly lists antigens required by law.
Excerpt from the regulations:
"... The test cells shall have the following characteristics: C, Cw, c, D, E, e, K, k, Fya, Fyb, Jka, Jkb, S, s, M, N, P1, Lea, Leb. It is recommended that the following traits are present in high antigenic density (homozygous inheritance for the allele) on the test cells: D, c, Fya, Fyb, Jka, Jkb, S, s."
Either two or three cells are used and the same procedure is followed as for the reverse typing. First, test cells are placed in the well, then the patient's serum (or plasma) - incubate - centrifuge - interpret.
It is common to perform the reverse typing along with the antibody screening test. In both examples, two cells are used for the screening. In the left picture, the screening is positive (all test cells have reacted with an antibody and remained on the gel during centrifugation). In the right picture, however, the two test cells (I, II) are all at the bottom of the well - indicating that there were no antibodies to react with the cells.
If the serum examined in the picture on the right belongs to our patient, then we have now determined the complete blood group. And it is:
B Rh pos, no irregular antibodies present
In the left scenario, the test for antibodies came back positive. In this case, further testing needs to be done to identify the specific antibodies present. It's interesting to note that the O cell also tested positive. Without this cell, the blood type would be O, but because the O cell reacted strongly in the reverse typing, the Bombay type is possible, although this is very unlikely. It's more probable that one or more irregular antibodies are present, possibly caused by previous immunization through transfusion or pregnancy. The two cells in the antibody screening test also reacted strongly positive. To determine the blood group in this case, the specific antibodies need to be identified through an antibody identification test.
Updated on 02.07.2024